Non-invasive Temporary Pacing
Non-invasive temporary pacing (NTP), an accepted emergency intervention since 1982, has been shown to be safe and effective over the ensuing years. It is considered to be a “tried and true” treatment modality, so little is written about it today. Even the American Heart Association (AHA) includes it as an integral step in the ACLS bradycardia algorithm.1 Most of the papers underlying the scientific basis for the practice of NTP were published in the 1980s and 1990s, with only a few advances coming to the forefront these last years.
What Is Non-invasive Temporary Pacing?
NTP is the technique of electrically stimulating the heart by use of a set of pads placed externally on the torso. ECG electrodes are also placed on the patient to sense ventricular events (spontaneous or paced), and the pulse generator delivers a wave pulse when a predetermined escape interval has elapsed. The stimulus is intended to cause cardiac depolarization and subsequent myocardial contraction. NTP is a method to secure cardiac pacing quickly and effectively until a transvenous pacemaker can be inserted or the condition necessitating pacing resolves.
Non-invasive Cardiac Pacing
The concept of non-invasive cardiac pacing has been known for about 200 years. In 1791, Galvani reported that an electrical current applied across the heart of a dead frog resulted in myocardial contraction. However, non-invasive pacing was not made practical until Dr. Paul Zoll's work in the early 1950s. In 1952, Dr. Zoll reported the successful use of subcutaneous (beneath the skin) needle electrodes in pacing two patients with ventricular standstill. He later reported the development and successful use of the first true, non-invasive pacemaker and monitor. This device used a pair of 3-centimeter metal electrodes secured to the chest wall and delivered 2-millisecond, 120-volt, alternating current (AC) impulses. Dr. Zoll is the acknowledged father of external pacing.
Technological improvements during the late 1980s made non-invasive pacing more comfortable and less cumbersome than earlier efforts. In 1981, ZOLL Medical Corporation patented and introduced a non-invasive external pacemaker with a longer pulse-duration (40 milliseconds) and a larger electrode surface area (80 cm2). This reduced the current required for capture and increased comfort for the patient. Additionally, this model could be applied more rapidly than earlier non-invasive pacemakers, renewing clinical interest in non-invasive pacing.
In 1982, the FDA approved the use of the ZOLL non-invasive pacing technology for patients with heart rates of less than 40 beats per minute and asystole (absence of electrical and mechanical activity in the heart). External pacing was found useful as a temporizing measure in patients with symptomatic bradycardia (a slower heart rate) and a pulse. The American Heart Association’s Advanced Cardiac Life Support (AHA's ACLS) Guidelines recommend non-invasive pacing as a temporary treatment for symptomatic bradycardia and as a consideration for asystole. Non-invasive pacing is a Class IIA recommendation for symptomatic bradycardias by the American Heart Association.
Non-invasive Pacemakers
An artificial pacemaker is an electronic device that provides an electrical signal to make the heart beat when the heart's own built-in pacemaker, or conduction system, fails. The body’s anatomical, built-in pacemaker, known as the SAN (Sinoatrial) node is made up of specialized nervous tissue at the junction of the superior vena cava and the right atrium. When the SA node generates an electrical impulse, it causes the heart to contract, and the right and left atria carry the signal on to the atrioventricular (AV) node. The AV node then carries the impulse through the wiring in the ventricles, thus causing the lower chambers of the heart to contract. The anatomical pacemaker provides what is called the heart’s “intrinsic” rhythm. When the internal pacemaker fails or is compromised, artificial pacemakers are appropriate therapy.
There are two types of artificial pacemaker: temporary and permanent. Permanent (epicardial) pacemakers are implanted by means of a surgical procedure and are used to treat permanent conduction problems. Temporary pacemakers are used in emergency situations for transient conduction disturbances or prophylactically for anticipated dysrhythmias. Temporary pacemakers may be invasive (transvenous) or non-invasive (transthoracic). Temporary non-invasive pacemakers are typically available to clinicians as part of a cardiac resuscitation system, complete with defibrillation, cardioversion, and monitoring capabilities.
Indications for Non-invasive Pacing – Maintaining Cardiac Output
The two most common reasons for using temporary pacing to maintain an optimal cardiac output are when the patient has developed a symptomatic bradycardia or is asystolic.
The cause for this is frequently due to impairment within the conduction system in the heart. The problem may be located within the atrioventricular (AV) node or below, within the bundle branches coursing through the ventricles. Patients can experience bradycardia as a result of several types of AV blocks. This, in turn, frequently causes decreased cardiac output. Permanent pacemakers can be implanted into these individuals to increase and maintain adequate heart rate.
A second reason patients may require temporary pacing is because they are experiencing fast heart rates. Symptomatic tachycardias (rates greater than 180) may produce inadequate ventricular filling with inadequate perfusion. Some very chaotic rhythms, like ventricular fibrillation, require defibrillation. Some fast rhythms (tachycardia) are amenable to overdrive pacing by a pacemaker. These may be atrial tachydysrhythmias (atrial flutter, atrial fibrillation, or atrial tachycardia) or ventricular tachycardia. This rapid rate may impair the ability of the heart to eject an adequate stroke volume. A temporary non-invasive pacemaker can be used to pace the atria at a rapid rate. If one of the pacer stimuli falls at the right time, it gains the responsibility for pacing the heart. This is known as overdrive pacing, and it either stops the tachydysrhythmia or converts the patient to a sinus rhythm.
Temporary pacing can be used either on an emergency basis or to support and/or maintain an adequate heart rate for several hours or days. In some cases, the clinician uses a temporary pacemaker until the patient is stabilized and definitive care, such as a permanent implanted pacemaker, is available.
Pediatric Pacing Indications
During the last decade non-invasive pacing has been an increasingly accepted therapy for adults and now, thanks to the availability of pediatric pacing electrodes, this therapy is feasible and practical for infants and small children as well.
Bradycardia is the most common dysrhythmia in children and is usually secondary to hypoxic (lack of oxygen in arterial blood) events. Although non-invasive pacing may be attempted, typically bradycardias of hypoxic origin do not respond to any therapies other than oxygen. First-line therapy is prompt airway support, ventilation, and oxygenation. Although less frequently than adults, children and infants do experience heart blocks and bradycardias in which treatment with non-invasive pacing is indicated and could be lifesaving.
Indications for pediatric non-invasive pacing include:
- Bradycardias from surgically acquired AV blocks
- Congenital AV block
- Viral myocarditis
- Newborn complete heart block due to maternal lupus
- Heart block secondary to toxin or drug overdose
- Permanent pacemaker generator failure in the pediatric patient with an implanted pacemaker.
Conditions in which non-invasive pacing is most often indicated include:
- Absolute bradycardia (HR < 30 bpm) with evidence of very low perfusion or frank shock (often associated with acute Myocardial infarction or cardiac ischemia involving the SA or AV nodes).
- Unstable or relative bradycardia as defined by these signs of inadequate perfusion:
- Altered mental status with poor perfusion
- Clinical signs of shock
- Severe shortness of breath/pulmonary edema
- Severe chest pain (consistent with ischemia)
- Inadequate skin perfusion with diaphoresis
- Cyanotic on 100% oxygen with adequate ventilation
- Asystole with a short time (< 10 minutes) since collapse, particularly if the asystole occurred shortly after defibrillation or medication administration
Non-invasive pacing is not likely to be effective in situations of prolonged duration of cardiac arrest.
Anterior - lateral placement requires little patient movement and allows for easy monitoring or defibrillation during transport.
The outcome of prolonged bradycardic or asystolic cardiac arrest is poor, even with non-invasive pacing. Indiscriminate pacing of this rhythm is unwarranted, particularly as a late effort in the resuscitation. Pacing of bradycardia or asystole of short duration, especially post counter-shock bradycardia/asystole, is more likely to be useful.
Non-invasive Pacemaker Functionality
The non-invasive pacemaker does two things: it monitors the patient’s own intrinsic rhythm using a “sensing circuit,” and it delivers an electrical signal using an “output circuit.” If the patient’s own intrinsic rhythm becomes too slow or disappears completely, the pacemaker senses the reduction in the signal or the rate and initiates pacing through the combination pads on the patient’s chest wall. The output signals provide a regular electrical stimulus to the heart’s conduction system, signaling the heart to contract at a rate determined by the pacemaker.
Pulse duration
Pulse duration is the time of impulse stimulation. Early non-invasive pacemakers used short-duration (1-2 milliseconds) impulses. The action potential (electrical impulse including depolarization and repolarization) of cardiac muscle cells is longer than that for skeletal muscle, requiring 20-40 milliseconds to reach maximum effect. ZOLL found that increasing the duration from 1 to 4 milliseconds resulted in a 3-fold reduction in threshold (the current required for stimulation) to produce capture. Increasing the current from 4 to 40 milliseconds further halves the threshold. Longer durations produced no further advantage. Current ZOLL non-invasive pacemakers deliver a 40-millisecond impulse for each paced beat. This 40-millisecond impulse is patented by ZOLL.
Synchronous/asynchronous modes
Most defibrillators have both fixed rate and synchronous pacing. Synchronous pacing is a demand mode, in which the pacer fires only when no complex is sensed for a predetermined amount of time. Pacing generally should be started in the synchronous mode to coordinate the efforts of the cardiac resuscitation system’s pacemaker with the patient’s own cardiac electrical activity. In the fixed rate (asynchronous) mode, the non-invasive pacemaker delivers an electrical stimulus at preset intervals, independent of intrinsic cardiac activity.
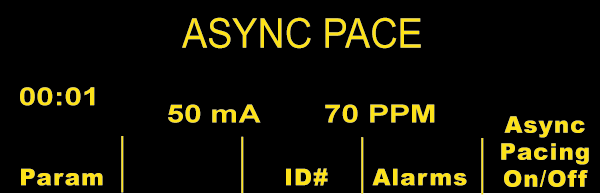
Asynchronous Pacing Mode
Current Requirements
Human studies have shown that the average current necessary for external pacing is about 65-100 milliamperes (mA) in unstable bradycardias and about 50-70 mA in hemodynamically stable patients and volunteers. The clinician increases the current until the pacemaker “captures” the myocardium, taking over the pacemaker functions of the heart and resulting in a characteristic pacemaker rhythm. The clinician then confirms the presence of a pulse following each pacemaker spike. The force of skeletal muscle contraction, not the electrical current, determines the patient’s level of discomfort during non-invasive pacing.
Electrodes
Non-invasive pacing can cause discomfort for patients and can be quite painful. Pain is a result of the current delivered per unit of skin surface area. Electrodes with a large surface area minimize pain sensation. Most commercially available electrodes are 80-100 cm2. Non-invasive pacemakers perform best with electrodes designed to function with that specific cardiac resuscitation system.
Proper application of the external pacemaker electrodes is simple but critical. Proper skin contact is an important factor in reducing resistance and improving capture.
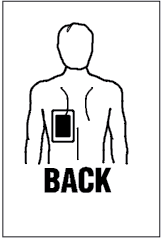
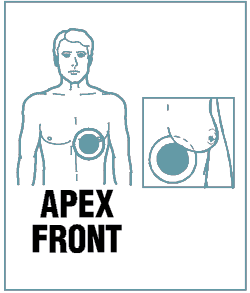
Posterior / Anterior
Anterior-posterior placement is preferred for external, non-invasive pacing. It may provide improved capture and will not interfere with defibrillation if required.
- Place negative electrode on left anterior chest halfway between the xiphoid process and left nipple, with the upper edge of the electrode below the nipple line.
- Place positive electrode on left posterior chest beneath the scapula and lateral to the spine.
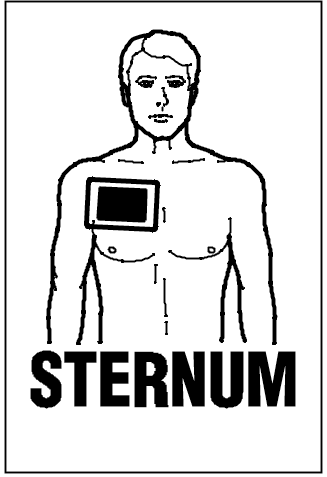
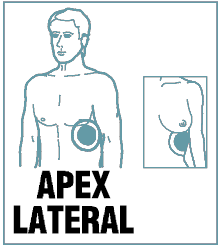
Anterior / Lateral
Anterior-lateral placement requires little patient movement and allows for easy monitoring or defibrillation during transport.
- Place negative electrode on left chest midaxillary around the fourth interspace.
- Place positive electrode on right chest, subclavicular area.
The current exits the negative electrode, travels through the heart causing depolarization of the myocardium, followed by ventricular contraction, and exits to the positive electrode.
Identification of mechanical capture
Mechanical capture manifests with signs of improving cardiac output such as an increased level of consciousness or blood pressure. The clinician must monitor and assess for both electrical and mechanical capture of the myocardium. The electrical activity of the external pacer shows up clearly on the monitor as large complexes at the rate you have selected. While pacing capture on the monitor is an important sign, the appearance of these complexes does not mean that the patient’s myocardium is mechanically captured and cardiac output is occurring.
The clinician must confirm that the heart is pumping and the cardiovascular system is generating blood flow by monitoring the pulse and not assume that the electrical activity of the pacer means that the heart is being paced.
Minimizing Discomfort
Skeletal muscle contraction can be uncomfortable and is often the limiting factor in non-invasive pacing use. Placing electrodes over areas of least skeletal muscle can minimize discomfort. The clinician should consider sedation if these measures are inadequate.