History and Science of Defibrillation
Since ancient times, humans have been curious about static shocks and the nature of lightning. In 1791, Luigi Galvani published his study of bioelectromechanics, including a notation that muscle contraction can be induced by electrical current. Overlooked was the idea that electrical current could be associated with the heart.1 Electrical current was mostly used to ensure that someone was really dead. In 1850, Karl Ludwig applied current directly to a dog’s heart and made it quiver.2 That raised a question: could electricity be used to stimulate the human heart?
In the late 19th Century, Battelli and Prevost found that weak current could cause ventricular fibrillation (VF) and stronger current could stop VF.3 Research in both the Soviet Union and in the U.S., with Gurvich and Yuniev proved direct current shocks stored in capacitors could successfully defibrillate dogs4, while Hooker and Kouwenhoven showed that defibrillation could take place without an open chest through work on accidental electrocution victims funded by the Edison Power Company.5 In 1956, Paul Zoll used the first alternating current defibrillator on a patient with syncope6 who was co-owner of Electrodyne, a small medical device firm.7 The AC defibrillator was used successfully between 1956 and 1961. In 1960, Bernard Lown introduced the first direct current (DC) defibrillator.8 The Lown waveform was the standard for defibrillation until the change to biphasic defibrillation, which started in the late 1980s.
Scientific Explanation of Defibrillation
Defibrillation is based upon the understanding that contraction of the heart, and the resulting circulation, is under the control of the heart’s electrical conduction system.
The sinoatrial node, (SAN) located within the wall of the right atrium, normally generates electrical impulses that are carried by special conducting tissue to the atrioventricular node (AVN).
Upon reaching the AVN, located between the atria and ventricles, the electrical impulse is relayed down conducting tissue (bundle of HIS) that branches into pathways that supply the right and left ventricles. These paths are called the right bundle branch (RBBB) and left bundle branch (LBBB), respectively. The left bundle branch further divides into two sub branches (called fascicles).
Electrical impulses generated in the SAN cause the right and left atria to contract first. Depolarization (heart muscle contraction caused by electrical stimulation) occurs nearly simultaneously in the right and left ventricles 1-2 tenths of a second after atrial depolarization. The entire sequence of depolarization, from beginning to end (for one heart beat), takes 2-3 tenths of a second.
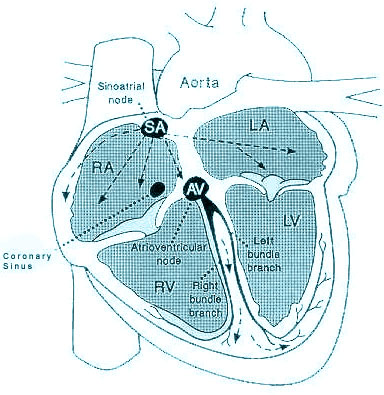
Should the SAN fail to produce impulses, the AVN can take over. The resting rate of the AVN is slower, generating 40-60 beats a minute. The AVN and remaining parts of the conducting system are less capable of increasing heart rate, due to stimuli previously mentioned, than the SAN.
Problems with signal conduction, due to disease or abnormalities of the conducting system, can occur any place along the heart's conduction pathway. Abnormally conducted signals, or arrhythmias, result in alterations of the heart's normal beating. This is visualized on the electrocardiogram (EKG).
Ventricular Fibrillation
Ventricular fibrillation (VF) is the most common electrical mechanism in cardiac arrest. Fibrillation is the manifestation of chaotic electrical excitation of the chambers of the heart. The consequence is the loss of coordinated contraction of the myocytes around the chambers so that the heart no longer pumps blood adequately or at all.
VF begins as a quasiperiodic reentrant pattern of excitation in the ventricles, with resulting poorly synchronized and inadequate myocardial contractions. Multiple foci within the ventricles are firing rapidly and independently. As the initial reentrant pattern of excitation breaks up into multiple smaller wavelets, the level of disorganization increases. There is no coordinated mechanical activity of the ventricles and, thus, no effective ventricular contraction.
The sudden loss of cardiac output with the subsequent tissue hypo-perfusion creates global tissue ischemia. The brain and the myocardium itself are most susceptible to the loss of oxygenation, and tissue death begins within minutes.
The Etiology of Ventricular Fibrillation (VF)
The etiology of VF is not completely understood. It often occurs in the setting of acute cardiac ischemia or acute myocardial infarction (MI). It is diagnosed in up to half of sudden-death survivors.
Abnormal rapid stimulation of the ventricles (ventricular tachycardia, or V-tach) can lead to fibrillation. Severe left ventricular dysfunction, a variety of cardiomyopathies, and acquired or idiopathic long QT syndrome also increase the risk of fibrillation.
Pathophysiology of VF
Sudden cardiac death can be viewed as a continuum of electromechanical states of the heart:
- Ventricular tachycardia, VT
- Ventricular fibrillation, VF
- Asystole or pulseless electrical activity (PEA)
VF/VT is the most common initial state, and due to insufficient perfusion of vital cardiac tissues, it degenerates to asystole if left untreated.
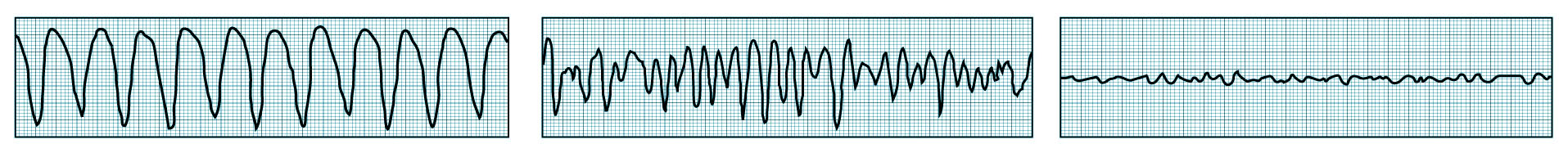
VF begins as a coarse, irregular deflection on the ECG, then degenerates to a fine, irregular pattern, and eventually becomes asystole, as shown in the following image.
At the onset of VF, the QRS complexes are regular, widened and of tall amplitude, suggesting a more organized ventricular tachyarrhythmia. Over a brief period of time, though, the rhythm becomes more disorganized, with high amplitude fibrillatory waves – this is coarse VF. After a longer period of time, the fibrillatory waves become finer, culminating in asystole.
The Progression from V-Tach to Fine VF
Defibrillation is the definitive treatment for the life-threatening cardiac arrhythmias, ventricular fibrillation, and pulseless ventricular tachycardia. Defibrillation consists of delivering a therapeutic dose of electrical energy to the affected heart with a device called a defibrillator. This depolarizes a critical mass of the heart muscle, terminates the arrhythmia, and allows normal sinus rhythm to be re-established by the sinoatrial node.
Defibrillators can be external, wearable, or implanted, depending on the type of device used, but all operate on the same principle. A ventricular arrhythmia is detected by the monitoring circuit of the device. A capacitor is charged with an appropriate level of voltage for the device (either by an operator or automatically) and upon initiation of the shock (automatically or upon the press of a button) current is delivered directly to the heart to interrupt the arrhythmia and restore normal conduction. When the current is delivered via an internal defibrillator far less current is required as there is not a lot of resistance in the circuit. External defibrillators, however, have to be able to deliver sufficient current to reach the heart through the mass of skin, hair and tissue.
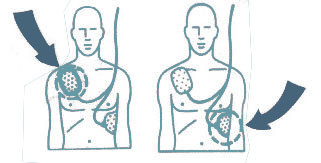
Previously most external defibrillation shocks were delivered via paddles placed upon the patient’s chest and the waveform was monophasic; current traveled in one direction through the heart (monophasic waveform). Two major changes have occurred in the past decade. Today in the U.S., the majority of defibrillation shocks are delivered through defibrillation electrodes, pads that are placed directly on the patient’s skin. These defibrillation pads are safer for rescuers, and because they conform to the chest are generally able to deliver the current more effectively.
The second major change in defibrillation is the use of biphasic waveform to deliver the current to the heart. With a biphasic waveform, current is delivered to the heart in two vectors. Because of the two-vector approach, the peak current required to convert the arrhythmia is reduced, and the efficacy of the shock is greatly enhanced. It is generally accepted that biphasic defibrillation results in less myocardial damage from the shock itself.
1. Galvani LA. De viribus electricitatis in motu musculari: commentarius. De bononiense Scientiarum et Artium Instituto atque Academia Commentarii. 1791;7:363-418.
2. Roth N. First stammering of the heart: Ludwig’s kymograph. Med Instrum. 1978;12:348.
3. Beck CS. Prevost and Battelli. Ariz Med. 1965;22:691-694.
4. Gurvich NL, et al. restoration of a regular rhythm in the mammalian fibrillating heart. Am Rev Soviet Med. 1946;3:236.
5. Hooker DR, Kouwenhoven WB, et al. The effect of alternating electrical currents on the heart. Am J Physiol. 1933;103:444-454.
6. ZOLL PM, et al. Termination of ventricular fibrillation in man by externally applied electric countershock. NEJM. 1956; 254:727.
7. Cohen S. Paul M. Zoll, MD—The Father of “Modern” Electrotherapy. Resuscitation. 2007;73:178-185.
8. Lown B, et al. Comparison of alternating current with direct current electroshock across the closed chest. Am J Cardiol. 1962;10:223.