Manual CPR
Manual CPR was developed in the late 1950s, and in 1960 the American Heart Association (AHA) began to teach physicians to use the technique. Over the next decade the technique was refined and taught to professional and lay rescuers worldwide.
Despite widespread education, the outcomes from sudden cardiac arrest have not improved significantly since the 1960s. Beginning with Paradis’ groundbreaking work on coronary perfusion pressure and its relationship to achieving return of spontaneous circulation (ROSC), clinical researchers have studied manual CPR, and today there is a body of evidence that shows how CPR performance affects perfusion, ROSC, and ultimately outcomes.1 This information is summarized below.2
The AHA recognizes that there are five critical components to high-quality CPR.
- Perform chest compressions at a rate of 100-120/minute.
- Compress to a depth of at least 2 inches (5 cm) but do not exceed 2.4 inches (6 cm).
- Allow full recoil after each compression. No leaning.
- Minimize interruptions in compressions to less than 10 seconds with a goal of chest compression fraction as high as possible; a target of at least 60% (it may be reasonable with sufficient rescuers to achieve greater than 80%).
- Avoid hyperventilation (1 breath every 6 seconds).
Depth of Compression
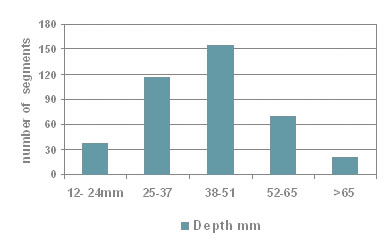
Abella et al. analyzed the measured depth of compression during in-hospital cardiac arrest and demonstrated a wide variation in compression delivery measured in 30-second segments.3
Mean Compression Depths for In-Hospital CPR
(Abella BS, Proceedings of ERC Symposia: Squeezing High Performance Out of CPR Medcom. 2006)
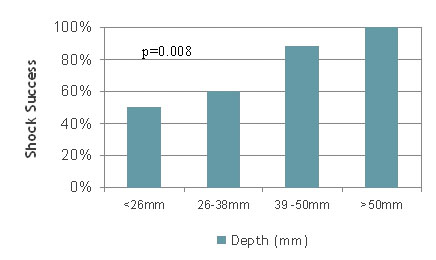
The group then studied whether the variance in compression depth was meaningful. Edelson reported the findings, which correlated depth of compression with shock success and determined that shock success correlated significantly with compression depth.4
Rate of Compressions
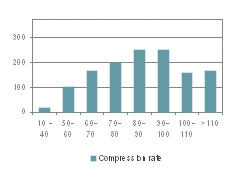
Abella et al. also measured the compression rate in 1626 30-second segments of CPR in three hospitals. In the study, rates were between 90 and 110 in only 36.9% of the segments.5
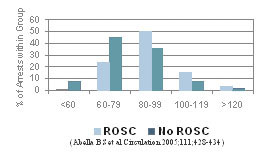
Abella et al. then correlated the rate of compressions with ROSC and found that overall, when ROSC was achieved, the mean compression rate was 90 + 17 compressions per minute (cpm)—near the recommended mean.5
With no ROSC, the rate was 79 + 17 cpm. The differences were significant, with a p value of 0.0033.
Interruptions in Compression
Wik et al. published a study in JAMA that found in 176 out-of-hospital arrests, chest compressions were being performed only about half of the available time, e.g., 50% of the time there was no flow.6 Furthermore, only 15%-20% of the no-flow time could be attributed to defibrillator use and required pulse checks. Additionally, interruptions for intravenous line placement and intubation, which occurred within the first five minutes of advanced life support (ALS), could not explain the ongoing no-flow periods.
Abella et al. reported that during in-hospital arrests, 40.3% of all the measured segments had no-flow intervals greater than a fraction of 0.20.7
Tang et al. demonstrated that rescuer fatigue impacts CPR quality, with CPP falling as time progressed over a 90-second period.8 With only 10 seconds of interruption—as rescuers were changed—the CPP fell significantly and getting back to optimal took a full minute. By this time, fatigue starts to impact quality once again. This does not take into account other interruptions for intubation, pulse checks, and such.
Ventilation
Aufderheide et al. demonstrated that during out-of-hospital rescues the frequency of ventilation averaged 30 times per minute.9 Abella et al showed a similar effect for in-hospital rescues, noting ventilation rates greater than 20 times per minute in 60.9% of the CPR segments measured.10
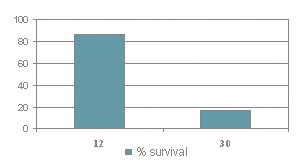
Pigs ventilated at a rate of 12 breaths per minute had a survival rate of 86% vs. those ventilated at 30 per minute had only 17% survival.
The foregoing clearly indicates that CPR quality plays an important role in resuscitation and that achieving the quality required is difficult.
Cheskes et al. concluded that pauses in CPR before a shock significantly impact survival to discharge.11 Every 5 second increase in pre-shock pause resulted in an 18% decrease in survival to discharge.
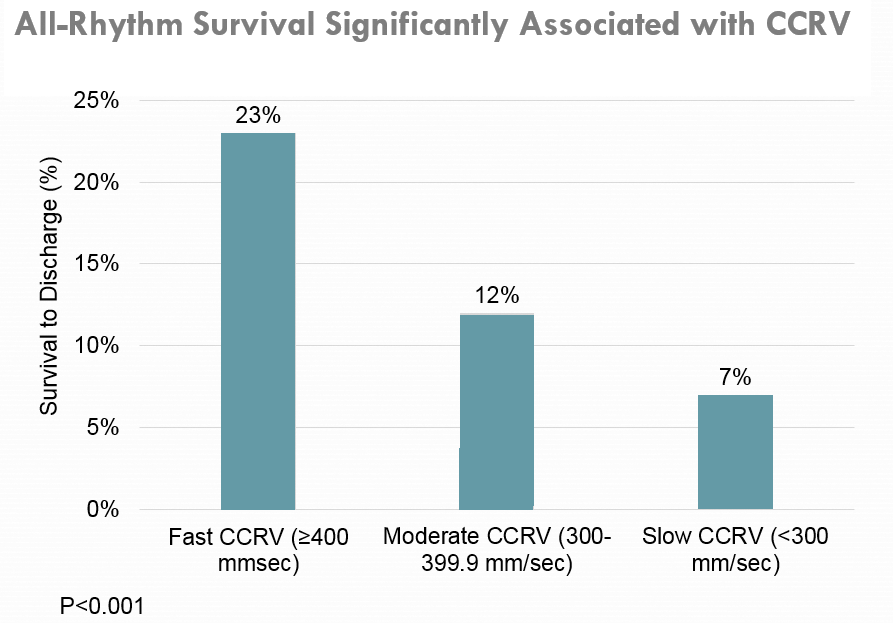
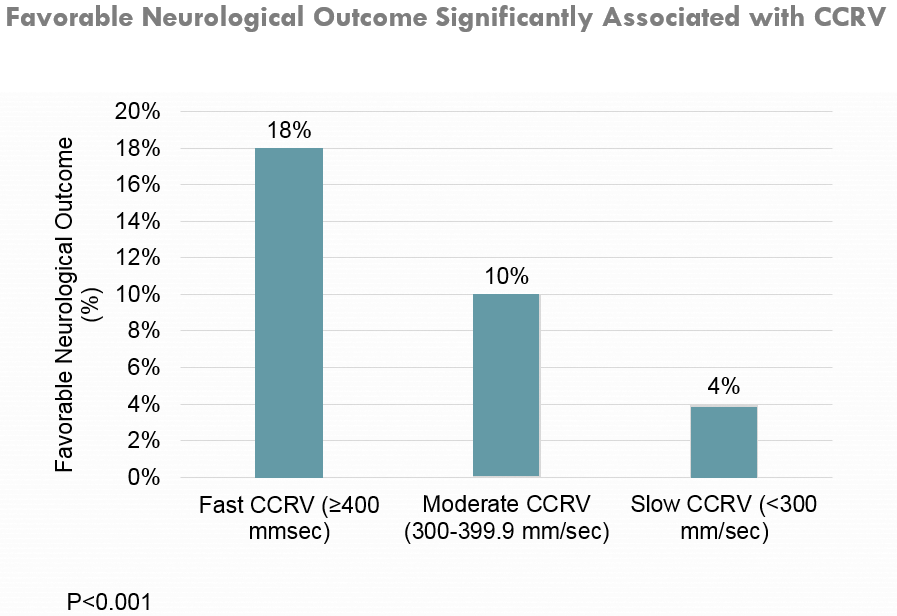
Release Velocity during Compressions
Kovacs et al. evaluated release velocity during the decompression phase of CPR and found that it was independently associated with improved survival and favorable neurologic outcome at hospital discharge after adult OHCA.12 A release velocity of over 400 mm/sec showed a 4-fold greater survival than release velocity of under 200 mm/sec and favorable neurological outcomes.
Tools to Improve Performance
There are several tools to assist rescuers when performing CPR. Stand-alone devices prompt users for appropriate rate and depth. The simplest is a musical metronome set to 100 beats per minute.
Three defibrillator manufacturers also offer tools for the defibrillator. Philips sells Q-CPR™, developed by Laerdal, for use with its MRx defibrillators. Physio-Control offers a feedback tool called TrueCPR™. These stand-alone sensors coach compression rate and depth when used during a rescue.
All of ZOLL's defibrillators offer Real CPR Help®, coaching tools that are integrated into the resuscitation electrodes and help rescuers achieve the correct rate and depth. In addition, the professional defibrillators, including the ZOLL R Series, X Series, and AED Pro, provide ECG filtering (See-Thru CPR®), which allows rescuers to see an organized rhythm without the need to pause compressions, reducing interruptions.
Note: It is not the intent of this site to teach CPR; use the Resources section to locate CPR training courses and guides.
1. Paradis, et al. Coronary Perfusion Pressure and the Return of Spontaneous Circulation in Human Cardiopulmonary Resuscitation. JAMA. 1990; 263(8):1106-1113.
2. Neumar, RW. Part 1: Executive Summary. 2015 American Heart Association Guidelines Update for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care. Circulation. 2015.
3. Abella BS, Proceedings of ERC Symposia: Squeezing High Performance Out of CPR. Medcom. 2006.
4. Edelson, et al. Resuscitation. 2006;71:137-145.
5. Abella, et al. Circulation. 2005;111:28-434.
6. Wik, et al. JAMA. 2005;293:299–304.
7. Abella, et al. Circulation. 2005;111:428–434.
8. Tang W. Go with the Flow: Proceedings of the ERC Symposia: Squeezing High Perfor¬mance out of CPR. Medcom. 2006.
9. Aufderheide, et al. Circulation. 2004;109:1960–1965.
10. Abella, et al. JAMA. 2005;293(3):305–310.
11. Cheskes, et al. Perishock Pause: An Independent Predictor of Survival From Out-of-Hospital. Circulation. 2011;124(1):58-66.
12. Kovacs, et al. Chest compression release velocity. Resuscitation. 2015;92:107–114.