Automated CPR
There are many challenges that inhibit providers from performing high- quality CPR on patients. Fatigue, moving patients from the scene of event to an ambulance, and delivering CPR in the back of an ambulance are a few of the reasons why the 2015 AHA Guidelines have recommended the use of automated CPR. In an attempt to overcome these difficulties, researchers and device manufactures began developing automated CPR devices in the 1990’s.

This device is manually set by the rescuer to deliver a fixed depth of compression. The device can be set to comply with the Guidelines 2015, and there is an optional hands-free ventilation capability. The current models include the LifeStat 1008 and the Thumper 1007C.
Similar in operation to the Thumper is the LUCAS device, as seen below, originally developed by JoLife. Also pneumatically driven, the LUCAS 3 is the most current version. The original model was operated by compressed air, while LUCAS 2 was electrically powered.

The third automated device is different from the previously mentioned devices. The ZOLL AutoPulse® is a load-distributing band compressor that is mechanically actuated and battery driven. AutoPulse provides both direct compression and semi-circumferential thoracic compression. It automatically sizes the patient and operates in both 30:2 and continuous compression modes and can be used at a 45-degree angle.
Effectiveness Data

The key is that these devices must perform at the same consistency as manual CPR and in the case of the AutoPulse, as high-quality CPR. In 2015, the AHA recognized the limitations manual CPR has in certain situations.3
Beyond the randomized trials, there is a significant amount of clinical data available, particularly with the AutoPulse. The following is a summary.
A Pilot Study in EMS with LUCAS
Axelsson et al. reported on a non-randomized controlled trial that evaluated the clinical consequences of the introduction of mechanical CPR in the EMS system for treatment of cardiac arrest.4 Patients included in the study all had experienced arrests. Exclusions from the trial included those under age 18, those undergoing trauma, pregnancy, hypothermia, intoxication, and hanging or drowning. Also excluded were those who experienced ROSC prior to the ALS unit arriving.
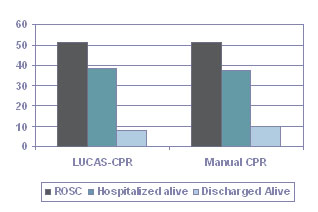
In the study, 105 patients were treated with LUCAS CPR and 169 patients with manual CPR. The median delay from onset of arrest to the arrival of the ALS unit was 12 minutes. When all patients were included in the analysis, there was no significant difference between the groups with regard to ROSC, survival to hospital admission or to hospital discharge.
The results for the LUCAS were then compared with a matched control population according to age, initial rhythm, witnessed status, etiology, and delay to start of CPR. Again, no difference was found among the groups in any of the variables evaluated. (P values for this study were under 0.20 and not statistically significant.) Authors of the study noted that a critical issue within the study was the way in which patients were randomized and the delay in intervention.
AutoPulse Studies
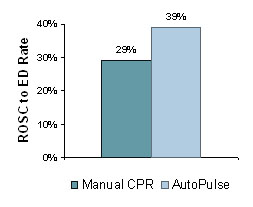
Two studies compared patients treated with manual CPR to patients treated with AutoPulse to determine the impact of AutoPulse on the delivery of patients with sustained ROSC to the emergency department (ED).
Casner et al. at the San Francisco Fire Department conducted a retrospective, case-matched review of the impact of the AutoPulse on survival.5
Specifically, the rate of delivery of 162 patients with ROSC to the ED was measured. The increased ROSC rate (35%) in the AutoPulse group was most pronounced when the initial presenting rhythm was asystole or pulseless electrical activity. (See Figure "ROSC to ED Rate.")
Casner M et al. Prehospital Emergency Care. 2005;9(1):61-67.
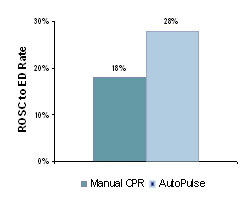
The major finding in this study was that the AutoPulse improved the rate of delivery of patients in ROSC sustained to the ED by 56%. Increased sustained ROSC rate was most pronounced when the initial presenting rhythm was asystole or PEA. Six survived greater than one year post arrest, five were neurologically normal. None of the subjects with manual CPR survived. AutoPulse produced pre-arrest levels of blood flow to the heart and brain (ACLS protocol – with epinephrine) and produced better EtCO2 results than manual CPR, and these results improved over time.
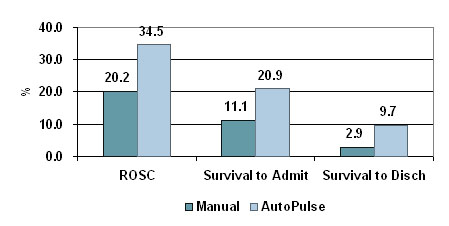
Ong, Ornato et al. at the Richmond Ambulance Authority in Virginia recently reviewed survival rates in 783 patients, 499 of whom had been treated with manual CPR and 284 who had been treated with the AutoPulse.7
Using AutoPulse, there was a 235% improvement in survival to discharge, 88% improvement in survival to hospital admission and 71% improvement in field ROSC. All results were statistically significant.
Virtually all the evidence supports the effectiveness of the AutoPulse device in increasing perfusion pressure, ROSC, and long-term survival rates.
1. Rubertsson, et al. Mechanical chest compressions and simultaneous defibrillation vs. conventional cardiopulmonary resuscitation in out-of-hospital cardiac arrest; The LINC randomized trial. JAMA. 2014;311(1):53-61.
2. Wik, et al. Manual vs. integrated automatic load-distributing band CPR with equal survival after out of hospital cardiac arrest. The randomized CIRC trial. Resuscitation. 2014;85(6):741-8.
3. Neumar, RW. Part 1: Executive Summary. 2015 American Heart Association Guidelines Update for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care. Circulation. 2015.
4. Axelsson, et al. Resuscitation. 2006;71;47-55.
5. Casner, et al. Prehospital Emergency Care. 2005;9(1):61-67.
6. Swanson, et al. Circulation. 2006;114(18):II-554.
7. Ong ME, Ornato J, et al. JAMA. 2006;295(22):2629-2637.